Feeling tired all the time led me to discover I had a vitamin D deficiency
I always knew I wanted to become a doctor but upon completing my education, my journey was anything but easy.
I had long commutes, sometimes a total of 150 miles in a day - but what's worse is that there would be days I’d drive to work in the dark and by the time I'd finish my work, the sun would have already set, leaving me to return in the dark too.
After a few years, I finally moved to a new practice closer to home and training life was better. It was January and my workday would start at 7 AM. If I was lucky, I would finish 12 hours later at 7 PM. The schedule was clear—sleep six hours, commute two hours round-trip, work 11 hours, study three to four hours.
Previously, in between the amount of stress of exams and working all day—I was heavily involved in sports (captain of her volleyball team) and extracurricular activities throughout. Tiredness, or being tired had never been a possibility, let alone in my dictionary. But now, I was finding it hard to stay awake.
If people living in countries on the equator like Pakistan, Dubai or Saudi Arabia complain about the heat, those from the north of the equator always long for the sun.
For the past six years, I had been living in a country where adequate sunshine was only between March to September. And before you think it doesn’t apply to you because you live in Pakistan—think again.
Even on days when I had slept enough, I wanted to sleep more. It wasn’t just feeling the need to sleep all the time, but constantly feeling exhausted and fatigued every single day. I was somehow still managing to do my work and studying, but my body felt like it would give up any time.
I then contacted my GP who 'investigated' the reasons for being “tired all the time”.
When my blood results came back, everything was normal - except for my extreme deficiency in vitamin D.
However what surprised me was that the lack of how just one vitamin could make me feel the way I was feeling. Being a patient is truly, a humbling experience.
A common problem, often overlooked
This wasn’t something new. A vitamin D deficiency is a common condition we see.
For the past six years, I had been living in a country where adequate sunshine was only between March to September. And before you think it doesn’t apply to you because you live in Pakistan—think again.
Despite adequate amounts of sunshine, a recent study in Pakistan concluded that 53.5% had a vitamin D deficiency, 31.2% had insufficient vitamin D, and only 15.3% had normal vitamin D.
Another paper looking at cumulative overview between 2008-2018 stated similar results, 58.17 per cent of the population is vitamin D-deficient and 26.65 per cent is insufficient in vitamin D.
In short, it doesn’t matter whether you live in the UK or in Pakistan, people with insufficient exposure to sunlight and those with darker skin are at higher risk of a vitamin D deficiency.
You may recall the Fair & Lovely ads where people say, “Dhoop mai mutt jao, kaali ho jao gi” and then the “kaun karega shaadi?" (seems like this is an all-pass reason to try to stop women from doing anything, even going out in the sun), & their readily available solution in bleach creams and skin lightening lotions.
What no one tells you, is the health implication of a lack of vitamin D—a.k.a the one you get directly from the sun— and what happens when your body doesn’t get the necessary amount.
Why is vitamin D important?
Vitamin D is an enzyme that regulates the calcium and phosphate balance in our bodies. It is essential for our musculoskeletal health and bone and muscle integrity.
A lack of vitamin D in children can cause a bone deformity called rickets, also known as bowed legs due to the permanent bending of the bones into a bow shape. In adults, it can lead to osteoporosis, where the bones become porous and brittle eventually leading to fractures.
Requirements
We obtain 90% of our vitamin D requirements through the synthesis in our skin, as a result of skin exposure to solar ultraviolet B (UVB) radiation. This is known as Vitamin D3.
The rule of thumb is 20–30min of sunlight exposure at midday to face and forearms, 3x per week, for adequate vitamin D synthesis in a fair-skinned young person. Elderly and dark-skinned require substantially more.
Vitamin D deficiency is actually very simple to prevent and treat. It requires you to take oral supplements at a high strength for a certain period of time before changing to a low dose. But the strengths are variable depending upon the regimes you follow.
The other 10% can be obtained through diet but mainly from animal sources such as: Oily fish (such as sardines, pilchards, herring, trout, tuna, salmon and mackerel), Egg yolk, red meat and liver, or fortified food (cereals) and fortified milk(not all countries add vitamins D to milk). obtaining vitamin D through dietary sources are difficult as they are limited and often do not faint the necessary daily requirements.
This obviously creates a dilemma for vegans and vegetarians.
Both forms, vitamin D2 and D3, require conversion in our bodies to their active forms.
What are the risk factors for developing a deficiency?
-Having dark skin — Asian, African, African-Caribbean, or Middle-Eastern ethnic origin fall into a high-risk category for not producing enough active vitamin D. This is due to the fact that melanin, the pigment that gives skin its brown or black colour, tends to absorb a proportion of the UVB radiation that is needed for vitamin D synthesis. Hence, they will produce less vitamin D as UVB light is dispersed.
-Those with limited sun exposure, for example, people who
a) cover their skin —which can be due to cultural reasons, for example as some Muslim women do, or for health reasons, e.g in those people with skin photosensitivity or history of skin cancer
b) people who generally do not spend time outdoors, e.g those who are housebound, or institutionalised
c) the amount can also be influenced by season, time of day, and weather conditions which vary from country to country. For example, from March to October, the solar UV levels are highest in the UK from 11 AM and 3 PM and are reduced by cloud cover. But during the winter, vitamin D is not synthesised.
Those with other non-variable risk factors such as:
-65 years and older are seen to have lower levels of serum 25-hydroxyvitamin D (25[OH]D) concentrations.
-Conditions that impair your body’s ability to absorb the vitamins and nutrients such as malabsorption syndromes e.g. Coeliac Disease, Crohn’s disease, Cystic Fibrosis as well as some Kidney and Liver diseases where Vitamin D is synthesised.
-Medications like corticosteroid (prednisolone), antiepileptics (gabapentin), laxatives (Senna), cholesterol-lowering drugs, tuberculosis medication (rifampicin) and weight loss medication can all impair absorption.
-Obesity itself is associated with lower vitamin D.
-Other factors such as cancers, family history of Vitamin D deficiency, and obesity can all negative impact the amount of Vitamin D in our bodies.
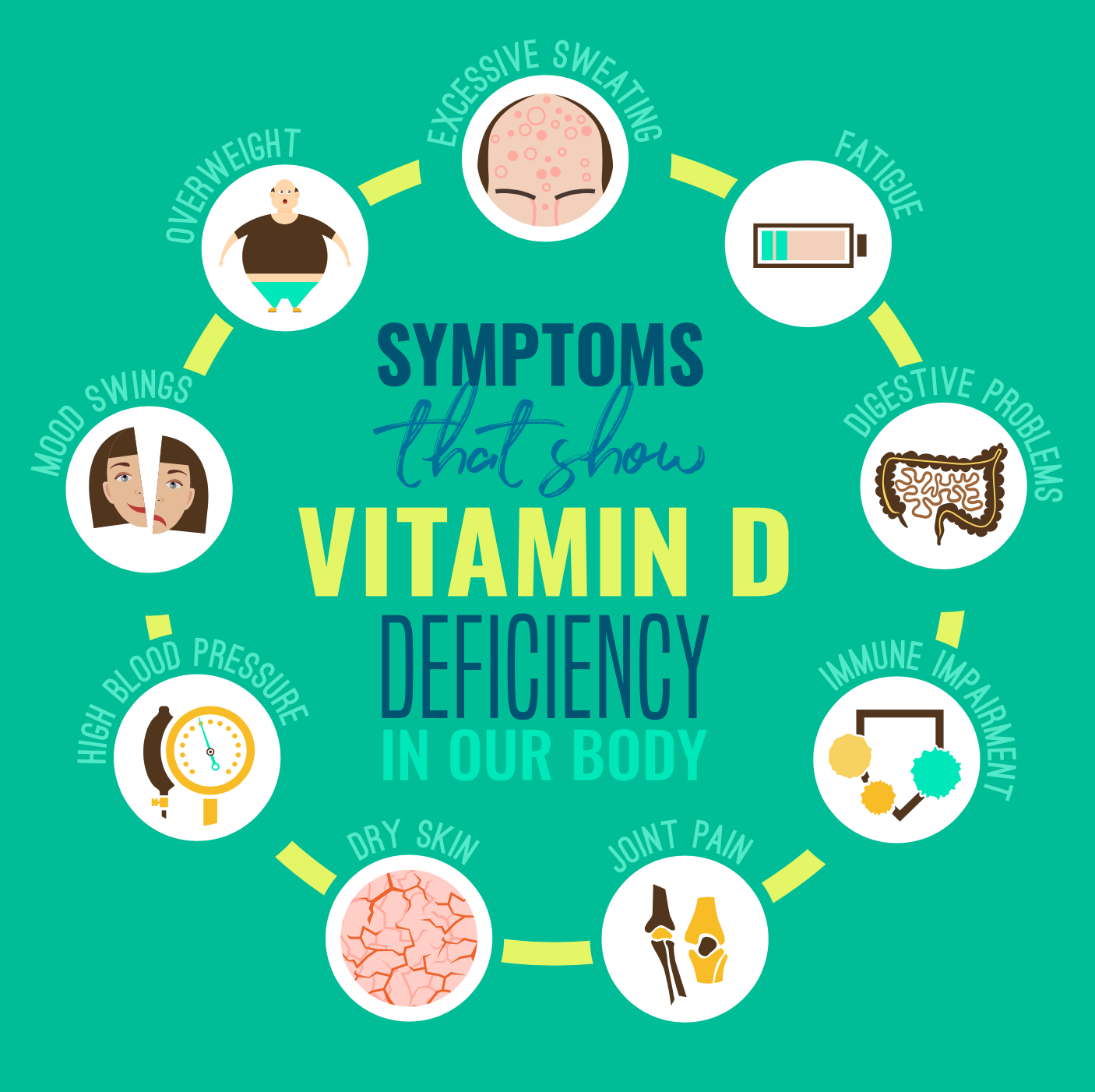
How might you know you have a vitamin D deficiency?
Symptoms in adults can be particularly vague which can make it difficult to diagnose as was the case with me.

Feeling fatigued, bone pain or tenderness, muscle weakness, mood changes like depression, and no other plausible explanation are all acceptable.
Ask yourself —
Have you been feeling tired and sleepy all the time?
Finding it difficult to do anything, noticing you’ve had muscle aches?
Can’t really tell what's wrong? If so, it may be worth having a chat with your doctor.
In children—
Symptoms can be even harder to identify in children.
While skeletal deformity, leg bowing or know knees may be obvious ones; other symptoms include tetany, irritability, impaired growth, muscle pain or weakness and bone pain.
If you are concerned, please consult your doctor who will suggest a blood test to detect vitamin D deficiency in the blood.
How can you treat it?
Vitamin D deficiency is actually very simple to prevent and treat. It requires you to take oral supplements at a high strength for a certain period of time before changing to a low dose. But the strengths are variable depending upon the regimes you follow.
National Institute of Care Excellence in England advises treatment of vitamin D deficient patients with oral vitamin D3 tablets. IM injections are available but are not recommended due to concerns regarding possible toxicity as well as uncertainty around their bioavailability.
Treatment is dependent upon how deficient a patient is, and may involve an initial high loading dose therapy regime, before continuing with low dose maintenance therapy.
Your doctor will advise you best regarding treatment for your specific case.
If you feel you have any symptoms or are worried, please consult your doctor.
Health risk advice
It is important not to overdose as taking too much can cause hypercalcaemia which can weaken the bones and damage the kidneys and the heart.
Sunscreen should STILL be worn at all times to protect one from premature skin ageing as well as decreasing chances of developing skin cancer.
Evidence identified by the Scientific Advisory Committee on Nutrition (SACN) suggests that although sunscreens can significantly reduce the production of vitamin D under very strictly controlled conditions, their normal usage does not generally prevent vitamin D synthesis.





Comments